Scars: In the Line of Tension
Marjorie Brook, creator of the Scar Tissue Release and Integrated Therapies (S.T.R.A.I.T Method™), speaking at the Polish Fascia Symposium on scar tissue.
I have been a massage therapist for over 20 years. In this time I have seen:
- Complications from scar tissue be dismissed by doctors – leaving their patients in pain and frustration
- A general population completely in the dark as to what is the root of their pain and suffering (i.e. they don’t realize that their back pain or shoulder pain is coming from the fall they had at the age of 15 that left a scar across their abdomen
- To current considerations by the medical profession that it may be a problem to some
Are Scars Really a Problem
This is a question I hear over and over and over again. And the answer is simply – while not every scar presents a problem, they all have the potential to become one.
Scars have been documented for over 3,700 years, yet they are still not entirely preventable. Despite advancement in the management of several diseases during the last centuries, scarring remains a tremendous clinical challenge to patients and clinicians.
Scar formation, although evolutionarily beneficial in wound healing, can create a substantial aesthetic and functional burden. And yet it is still the ugly step sister of the medical field. Never given the respect and understanding it deserves.
We are the only species that heals with a pathological scar. No other species has keloids or hypertrophic scars. Humans are a tight-skinned species unlike animals where the skin is loose for example a mother picking up her cub by the scrub of her neck. Our skin is very tight around our bodies. Scarring is a late evolutionary event that probably arose in response to a need, as hunter-gatherers, to heal quickly to avoid infection or detection by predators. We’ve evolved for speedy repair. And speedy repair is not necessarily quality repair.
Scar Statistics
- There are an estimated 12 million traumatic lacerations treated in the United States emergency rooms each year
- 250 million surgical incisions created worldwide every year
- 11 million burns severe enough to warrant medical treatment worldwide
- Every year 300,000 to 400,000 Americans approach their doctors to get their scars reduced
- Over $20 billion dollars are spent every year on the treatment and management of scars (this includes creams, lotions and therapies)
Scar Tissues Impact on the Body
Scar tissue forms after an injury, trauma, surgery, and, in some cases, disease. It can develop on the skin’s surface or internally. And, unfortunately, it’s the superficial scars or surface scars that concern people the most. They are concerned with how it looks and what it is doing to their appearance while they fail to focus on what the scar is doing to their body internally.
Scars are often considered trivial, but they can be disfiguring and aesthetically unpleasant and cause:
- severe itching
- tenderness
- pain
- sleep disturbance
- anxiety
- depression
- disruption of daily activities
The list of long-term complications is hefty and include:
PHYSIOLOGICAL
- nerve impingement
- pain
- numbness
- limited range of motion and flexibility
- postural misalignment
- muscle atrophy
- tissue hypoxia
- an increase in potential for future injury
PSYCHOSOCIAL
- development of post-traumatic stress reactions
- loss of self-esteem
- stigmatization
Depending on the way in which the scar tissue matures over time, these symptoms may not occur until years after the injury which is why the person at 40 years old with neck pain or back pain doesn’t relate it to the scar from when they were 15.
Scar tissue has the potential to affect every system in the body.
- Integumentary
- Muscular-skeletal
- Nervous
- Circulatory
- Lymphatic
- Respiratory
- Endocrine
- Urinary / Excretory
- Reproductive
- Digestive
- Polarity
Understanding how each of these systems can be affected by scar tissue can you unravel the mysteries of the pain and frustration you’re suffering, in some cases for years.
Emotional Impact of Scar Tissue
Physical scars cannot and do not show how much pain or suffering a person has experienced.
- Shock
- Guilt
- Failure
- Loss
- Detachment
- Trauma
- Anger and resentment
- Fear
- Low self-esteem
- Hopelessness/depression
- Disgust when seeing or touching the scar
- Sadness about the limits the scar places on everyday life
- Humor – yes, there can be funny stories behind accidents
The emotions surrounding the physicals scars can and do have a direct emotional and psychological effect. It can bring about significant self-image issues and lower self-confidence.
Research on the aftercare of burn survivors or those with severe facial scarring has proven this. The cases of patients with severe scarring suffering from depression (between 13-23% of cases) or post-traumatic stress disorder (between 13-45% of cases) have been documented.
Helping scar tissue mature and heal in conjunction with the body’s original state gives you the best chance to minimize and/or avoid these symptoms altogether.
Scar Tissue Awareness
The potential for scar tissue related complications, in general, has been ignored or viewed as having no consequence. It is time to bring scar tissue into the light.
Recognition of potential to disrupt the natural order of the body.
- It is very common that people with scars are frustrated and confused by the complications they experience
- People with scars have no idea that the pain, stiffness, decreased mobility, lack of sensation, and weakness are resulting from their scars
- Without an understanding of what is happening to them, they do not know to seek therapy. They are left to face a lifetime of pain and limitations
- The medical world needs to start recommending actual scar therapy not just hand out creams or lotions to deal with scar tissue
Preventing scar development at the onset of wound healing is the ultimate goal.
The external shape of human body is determined by the underlying bony skeletal framework, which the skin must cover. To conform to this complex shape, the skin must be both viscous and elastic to deform and return to its original shape. Mechanically, it needs to be both strong and flexible and scar tissue interferes with this. Scar tissue is only 70% as functional as normal tissue. So, it is not as strong as normal tissue, it is not as elastic as normal tissue and it will impede in the skin’s ability to reshape and reform around the skeleton which limits the range of motion, flexibility and causing other issues.
Scar Formation & Tension
It is a well-known surgical dictum that if wounds are closed under tension, scars stretch and worsen according to the magnitude and direction of the forces acting on them. In scar prevention, the single most important modifiable factor is wound tension during the proliferative and remodeling phases, and this is determined by the choice or incision design.
This brings us to the Langer’s lines, relaxed skin tension lines and biodynamic excisional skin tension or BEST lines. Most people do not consider these lines with scar tissue and how it affects it but it’s exactly what needs to be considered in both when it comes time to close the wound and for therapy thereafter.
LANGER’S LINES
Langer’s lines which are skin tension lines, or cleavage lines, are named after the Austrian anatomist Karl Langer who first depicted them.
- They are topological lines drawn on a map of the human body.
- They correspond to the natural orientation of collagen fibers in the dermis, and are generally perpendicular to the orientation of the underlying muscle fibers.
- Skin lines are important when making and closing wounds.
- Ideally all wounds should be made parallel to Langer’s lines to optimize the cosmetic outcome.
- Wounds made across the lines of skin tension promote hypertrophic scarring and by wounds we’re talking incisions made by doctors.
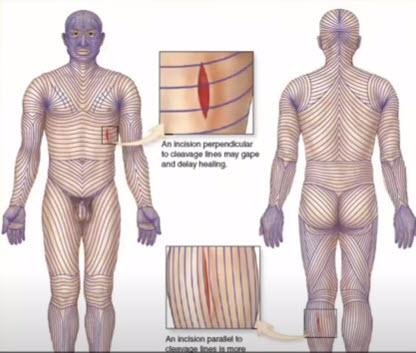
The photo illustrates an example to show you that an incision perpendicular to cleavage lines may deep and delay the healing due to the pull from the tension in that area as opposed to the lower one where the incision line is parallel to the cleavage lines and is more likely to heal quickly because it doesn’t have the same amount of opposing force or tension on it.
RELAXED SKIN TENSION LINES (RSTL)
Relaxed skin tension line (RSTL) is a furrow created when the skin is pinched and relaxed in the absence of local tension. Relaxed skin tension lines (RSTL) versus other skin lines. This is why we don’t have as much scarring with the elderly as the tissue is losing its elasticity and there’s not much tension on it. However, as we know because of the lack of collagen that we have the elderly bruising more.
When Langer’s lines and RSTL lines run in the same direction over many parts of the body they are significantly different in mechanically complex areas such as the mouth corner and the temple.
BIODYNAMIC EXCISIONAL SKIN TENSION (BEST) LINES
Biodynamic excisional skin tension (BEST) lines have been derived by using tensiometer data (measure of muscle force) from patients undergoing skin excision. These show the optimal orientation of a skin excision to minimize tension across its closure.
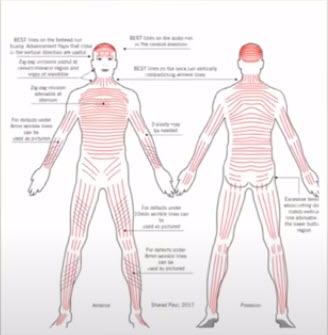
While Langer’s lines run in a sagittal direction on the scalp, BEST lines run in a coronal direction. While RSTL/wrinkle lines run in a horizontal-oblique directions or on the limbs. On the lower limbs, BEST lines run in a vertical direction. So we need to keep in mind what type of wound, how the wound was formed, what the shape of the wound is and where the location of the wound is.
When it comes to closing the wounds and when it comes to treating the wounds, BEST lines appear to have a remarkable anatomical consistency of pattern across the human body. Following BEST lines can therefore be expected to reduce wound tension and improve both cosmetic results and surgical outcomes.
Plastic surgeons follow these principles in order to minize scarring. Whenever possible the patient would be given the option to request a plastic surgeon to close the wounds and they need to be educated in regards to how to take care of the wounds after the surgery.
Post Injury Management of Surgical Incisions
The management of a surgical incisions does not end when the sutures are removed. Surgical scar care should be continued for one year. Scar tissue is continued to be produced for up to 18 months after the initial wound so just taking the sutures out because the surface is closed is not where the care should stop. We need to continue to treat and look after the area.
When an incision, cutting, ripping, or puncturing injury occurs the tension from the adjacent intact skin pulls the free edges of the wound apart. In places where the wounded skin is under greater tension, the wound gapes more widely and heals more slowly, and the resulting scar is relatively large.
Also, another consideration is that a new scar is weaker than the adjacent tissue. Scar tissue does not function the same as normal skin and if we have the newest scars or are the weakest in other words if you multiple scars you have one scar you go back for more surgery or you fall again in the same area. This new scar is not as strong and it’s weaker than the original tissue so you have multiple lines of tension being set up with different poles and different forces going against the original orientation and function of the skin. Pushes and pulls that would have no effect on healthy parts of the body can reopen a healing wound, even when it is protected by a well-made dressing.
Similarly, if there is significant skin tension surrounding the wound (e.g. over a bent knee), the healing wound will not be able to seal tightly. This is a big consideration for rehab for things like a knee or a joint. It’s usually common practice in physical therapy, at least old school, to force flexion on the knee very early into the healing process which doesn’t give the knee enough time to heal the area in order to avoid scar tissue. Unfortunately, force flexion causes more scar tissue because pulls and it helps pull the wound open during the flexion.
Phases of Wound Healing
You can’t talk about scar tissue and not talk about the phases of wound tissue.
Inflammatory Response
Occurs approximately 1 week to 30 days after surgery, when reparative cells gather at the incision, creating the structure on which future scar tissue will grow. It is perhaps the most vulnerable phase of scar formation.
Proliferative Phase
Cells divide rapidly to produce collagen, which fills gaps made by the incision, and worsened by everyday management and other stresses on the wound. It’s the time of greatest scar tissue growth, occurring until about 45 days after surgery.
Remodeling Phase
The critical end-phase of tissue healing, when the wound closes and fills with dry scar tissue. Gaps caused by tension on the skin may continue to be filled by collagen, leading to wider, thicker, darker scars, setting the stage for complete healing that may take up to a year.
Wound Healing Best Practices
Wound healing phases are not discrete. The proliferation phase begins even before the inflammation phase has completed and continues even as remodeling has begun. The remodeling phase itself continues long after the sutures have been removed and the dressing abandoned. Because of this, the care of an incisional wound should be considered as a continual process, and minimizing scar formation should be a long-term goal.
There are important aspects of wound management that must be emphasized to encourage patient participation.
Wounds should be dressed/taped following Langer’s to off load the tension. This would significantly reduce the scar.
- Gentle Movement: We have a tendency not to move to stabilize and isolate the area and leave it alone until the wound is closed and this is not the greatest thing in the world. As the wound heals slow gentle movement with intent to prevent restriction should be included in the therapy in order to encourage the collagen to lay down in the proper direction.
- Proper Nutrition: the vitamins and minerals that play roles typically associated with wound healing include vitamin A, vitamin C, zinc, copper and iron. Proteolytic enzymes can effectively “digest” scar tissue
Therapy for Existing Scars
Let’s talk about therapy for existing scars whether they’ve been around for 3 months or 80 years. The biggest and most important thing about treating scars is proper education.
I can’t stress this enough. The internet is now flooded with inaccurate information about scar tissue and ways to cure it. For example, that scar tissue cannot be broken down nor can it be removed. Anyone who claims to breakdown scar tissue, we’re not talking about adhesions, does NOT understand what scar tissue is. Scar tissue replaces normal tissue that is damaged. I you break it down or if your intent is to break it down you’re essentially saying that you’re going to cause a new wound. The only person who can actually remove scar tissue is a surgeon with a procedure such as scar revision. While scar revision removes the tissue usually results in the same or worse scar within a year after the procedure.
Once again we must return to the issue at hand – understanding and respecting scar tissue. Therapies are being applied with a total lack of understanding of the physiology of scar tissue. Many therapies look to interrupt and/or stop the formation of scar tissue before it has had time to complete its job – to repair and stabilize the wound.
Instead of trying to impede the formation we should be assisting and guiding it. Helping the collagen to laydown in a cohesive pattern. In order to do this, we once again must take the lines of tension into consideration. If it is a recent surgery all procedures should be looking at how the tensions have been altered from the wound and the client’s everyday living movement.
If it is an older wound, how has the formation of the scar tissue altered the tension in the body and how has the body compensated for it?
There is little, or worse, no knowledge behind the events that caused the scars (i.e. surgeries, accidents, and what the corrective procedures actually did to the body). I see this all the time. Scar tissue is very popular. We have all the tools such as cupping, instrument assisted blades, all types of therapies now but you can not just focus on the scar as an individual thing and go to release the scar.
You need to know the surgery behind it and everything that has occurred to that person via that surgery/accident, what was the rehab before you start to release that scar. For example, if you have someone who has had a mastectomy and reconstructive surgery, you need to know all the different types of reconstructive surgery, and the specific surgery that person has undergone. If they’ve had a piece of their lat removed, a piece of their glutes removed, if they’ve had the deep procedure. Any of those things and how all of those things have resulted in effects on the body both physically and emotionally. And remember the majority of people who get something like a reconstruction after a mastectomy do not receive rehab. And this is a very big problem.
We need to know how will releasing the scar affect the body – physically and emotionally. Little or no attention is paid to the physiological and emotional trauma surrounding the events which have caused the scar. So while working on the scar a person can have any possible emotional reaction during the treatment, after the treatment, within a week of the treatment, and not understand what is going on. So you need to make them aware of the fact and you need to be aware of the fact that this is a possibility so they are prepared to cope with it. Remember it’s not the issue in the tissue, the issue is in the brain. The tissue with the scar is the trigger.
What rehab has to be done after the release to aid the body to return to optimal function?
Few look for the possible compensations the body may have complied in response to the restrictions and what releasing those restrictions without proper rehab would do. You can not just release the scar and alter the tension that the body’s been working under and say “have a nice day.” We have to consider what has been altered and we have to figure out and work with the body to bring it back, as close as possible, to its original settings so the body can function in the manner in which it was designed. Otherwise, it’s going to go right back to what it knows which is the compensations that are in place.
As with all diseases, disorders, and dysfunctions (yes, scar tissue is/can be a cause of dysfunction), the therapist needs to understand all the aspects of what they are working with before they lay hands on someone.
There are so many wonderful forms of therapy available today to help people on their journey to balance health and wellness. No one is better than the other, rather we have to find the right one, or combination thereof, that works for each individual. That being said, there is nothing more important than recognizing the effect scars are having on a person. Knowing what those scars are doing physically, mentally and emotionally is key to helping a person heal.
In order for any therapy to be fully effective, you have to clear and release any and all scars that are impeding the body’s function. In other words, scar tissue release is the first step then you may proceed with any and all therapies that resonate with the patient.
Scars should not only be viewed as a symptom or end result of a wound/injury but as a cause/major factor in disease, disorders and pain.
》A B O U T M A R J O R I E B R O O K
 Marjorie Brook, LMT is a massage therapist, author and international educator. She works from the fundamental belief that your body is intuitively aligned with the thoughts you think, the emotions that you feel and the things that you do. She founded Brooks Seminars in 2007 after working as a decade as a nationally recognized massage therapist with a private practice on Long Island. She is the creator of the Scar Tissue Release and Integrated Therapies (S.T.R.A.I.T Method™) and offers continuing education courses on this method all over the world. Her articles have appeared in magazines such as Massage Today, American Fitness and Massage World. She’s approved by the National Certification Board for Therapeutic Massage and Bodywork, the Massage Therapy Association of Alberta and the College of Massage Therapists of British Columbia.
Marjorie Brook, LMT is a massage therapist, author and international educator. She works from the fundamental belief that your body is intuitively aligned with the thoughts you think, the emotions that you feel and the things that you do. She founded Brooks Seminars in 2007 after working as a decade as a nationally recognized massage therapist with a private practice on Long Island. She is the creator of the Scar Tissue Release and Integrated Therapies (S.T.R.A.I.T Method™) and offers continuing education courses on this method all over the world. Her articles have appeared in magazines such as Massage Today, American Fitness and Massage World. She’s approved by the National Certification Board for Therapeutic Massage and Bodywork, the Massage Therapy Association of Alberta and the College of Massage Therapists of British Columbia.
